TLDR The woman was diagnosed with lichen planopilaris and can be treated with corticosteroids.
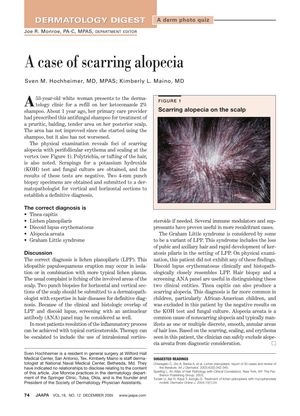
A white woman presented with a pruritic, balding, tender area on her posterior scalp that had not improved with ketoconazole 2% shampoo. Physical examination revealed scarring alopecia with perifollicular erythema and scaling. Negative KOH test and fungal culture results, along with two punch biopsies, led to a diagnosis of lichen planopilaris (LPP). LPP is an idiopathic condition that can be treated with topical corticosteroids, and in more severe cases, intralesional corticosteroids or immune modulators. Differential diagnoses included discoid lupus erythematosus, tinea capitis, and alopecia areata, but these were excluded based on clinical and histopathological findings.
 117 citations
,
March 2013 in “Journal of the European Academy of Dermatology and Venereology”
117 citations
,
March 2013 in “Journal of the European Academy of Dermatology and Venereology” No effective treatment for frontal fibrosing alopecia was found, but oral 5-alpha-reductase inhibitors had the best response; for lichen planopilaris, topical corticosteroids were commonly used but had a high relapse rate.
 January 2018 in “Elsevier eBooks”
January 2018 in “Elsevier eBooks” The document concludes that alopecia has various forms, each with specific treatments, but no definitive cure for certain types like CCCA has been proven.
 5 citations
,
November 2011 in “Expert Review of Dermatology”
5 citations
,
November 2011 in “Expert Review of Dermatology” The document concludes that early diagnosis and a comprehensive treatment plan are crucial for managing hair loss in children, with a focus on both medical and psychological support.
 4 citations
,
August 2010 in “Journal of the American Academy of Dermatology”
4 citations
,
August 2010 in “Journal of the American Academy of Dermatology” Cicatricial alopecia involves scarring hair loss and can be treated with various medications.
 May 2017 in “InTech eBooks”
May 2017 in “InTech eBooks” Some hair loss disorders cause permanent loss due to scarring, and treatments like steroids don't always work well.