Tinea Capitis Mimicking Dissecting Cellulitis of the Scalp: A Histopathologic Pitfall When Evaluating Alopecia in the Post-Pubertal Patient
December 2013
in “
Journal of cutaneous pathology
”
tinea capitis dissecting cellulitis of the scalp alopecia scalp erythema induration drainage hair loss biopsy inflammatory infiltrate PAS-positive spore oral terbinafine inflammation reduction hair regrowth punch biopsy fungal cultures KOH examination fungal stains superficial inflammation deep chronic inflammation scarring alopecia ringworm of the scalp terbinafine KOH test
TLDR A fungal infection can look like a different scalp condition in teens, leading to wrong treatment until proper tests are done.
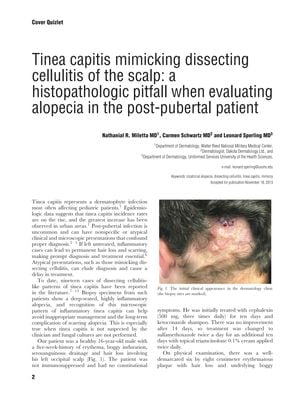
The document discusses a case where tinea capitis, a fungal infection typically seen in children, presented in an atypical manner in a 16-year-old male, mimicking dissecting cellulitis of the scalp. This uncommon presentation led to initial misdiagnosis and treatment failure. The patient had a five-week history of scalp erythema, induration, drainage, and hair loss, which did not improve with antibiotics and topical treatments. Biopsy revealed a dense inflammatory infiltrate, and a single PAS-positive spore was eventually identified, leading to the correct diagnosis of tinea capitis. The patient was then successfully treated with oral terbinafine, resulting in marked inflammation reduction and hair regrowth. The paper emphasizes the importance of considering tinea capitis in post-pubertal patients with inflammatory alopecia and suggests that a punch biopsy, fungal cultures, and KOH examination should be performed when the clinical presentation is atypical. It also notes that fungal stains are often negative in inflammatory tinea capitis, but careful examination may reveal fungal elements, and a pattern of both superficial and deep chronic inflammation should prompt a clinical reappraisal for tinea capitis to avoid long-term complications like scarring alopecia.





